-
Email Address info@triesencehcp.com
-
Phone Number 1-833-442-7769
-
Our Location
1A Burton Hills Boulevard
Suite 200, Nashville, TN 37215
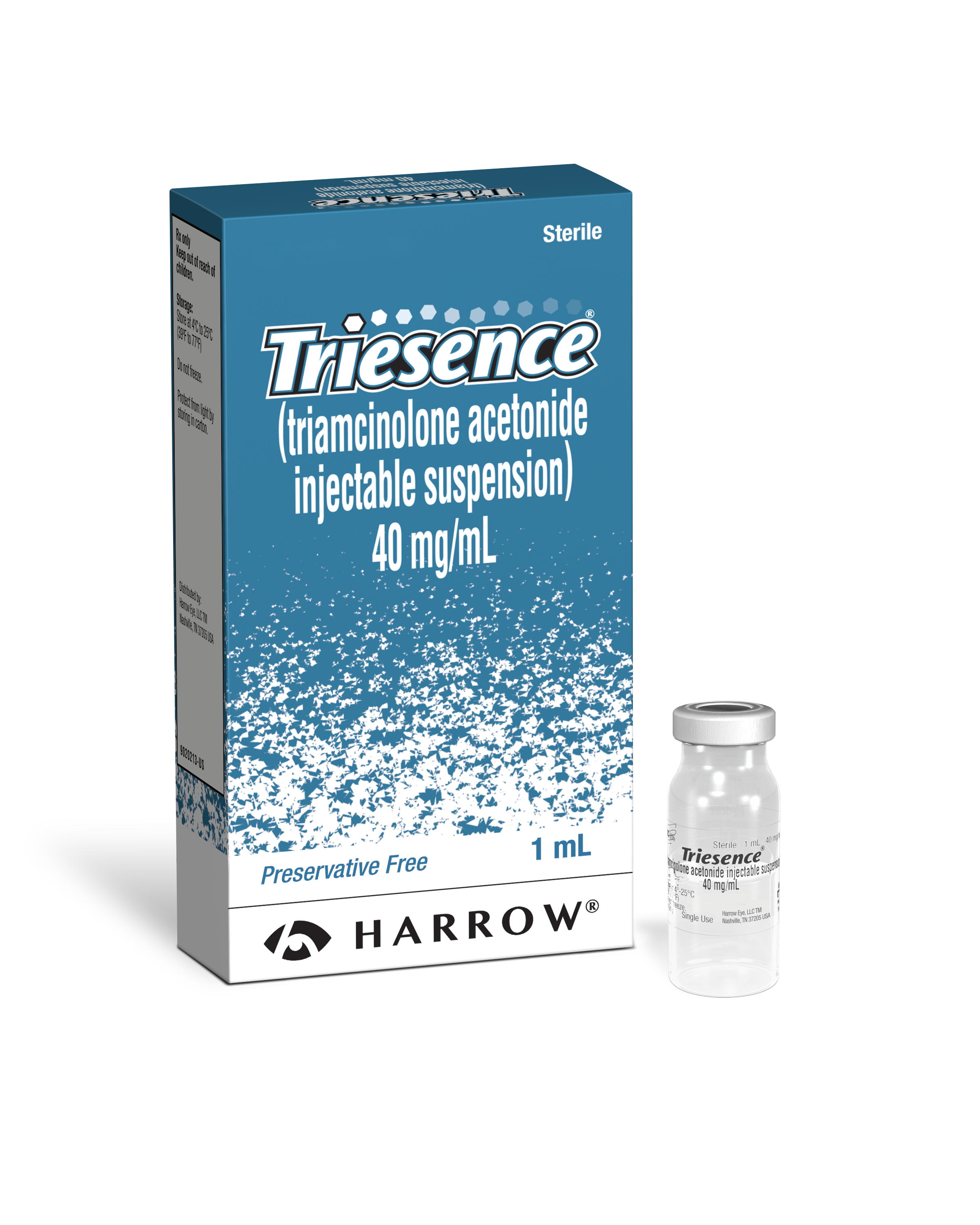
TRIESENCE®
Proven & FDA-Approved
The only preservative-free synthetic steroid that is FDA-approved for visualization during vitrectomy, uveitis, and for the treatment of ocular inflammatory conditions that are unresponsive to topical steroids.1
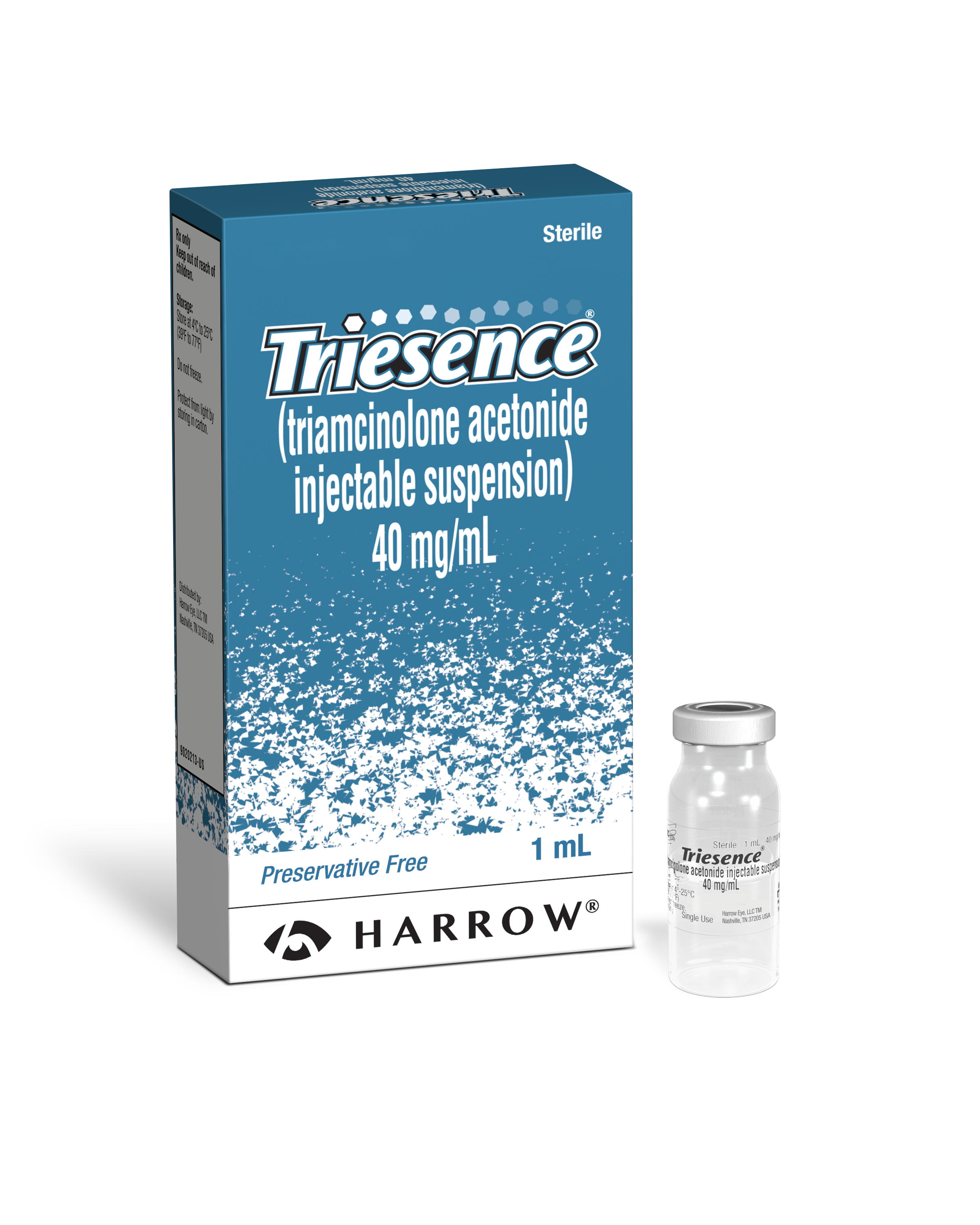
Proven & FDA-Approved

IMPORTANT SAFETY INFORMATION
INDICATIONS AND USAGE
TRIESENCE® Suspension is indicated for:
- Treatment of the following ophthalmic diseases: sympathetic ophthalmia, temporal arteritis, uveitis, and ocular inflammatory conditions unresponsive to topical corticosteroids.
- Visualization during vitrectomy.
- TRIESENCE® Suspension is contraindicated in patients with systemic fungal infections.
- TRIESENCE® Suspension is also contraindicated in patients with hypersensitivity to corticosteroids or any component of TRIESENCE® Suspension. Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy.
- TRIESENCE® is a suspension; it should not be administered intravenously.
- Ophthalmic effects: May include cataracts, infections, and glaucoma. Monitor intraocular pressure.
- Hypothalamic-pituitary-adrenal (HPA) axis suppression, Cushing’s syndrome and hyperglycemia: Monitor patients for these conditions and taper doses gradually.
- Infections: Increased susceptibility to new infection and increased risk of exacerbation, dissemination, or reactivation of latent infection.
- Elevated blood pressure, salt and water retention, and hypokalemia: Monitor blood pressure and sodium, potassium serum levels.
- GI perforation: Increased risk in patients with certain GI disorders.
- Behavioral and mood disturbances: May include euphoria, insomnia, mood swings, personality changes, severe depression, and psychosis.
- Decreases in bone density: Monitor bone density in patients receiving long term corticosteroid therapy.
- Live or live attenuated vaccines: Do not administer to patients receiving immunosuppressive doses of corticosteroids.
- Negative effects on growth and development: Monitor pediatric patients on long-term corticosteroid therapy.
- Use in pregnancy: Fetal harm can occur with first trimester use.
- Weight gain: May cause increased appetite.
- Based on a review of the available literature, the most commonly reported adverse events following ocular administration of triamcinolone acetonide were elevated intraocular pressure and cataract progression. These events have been reported to occur in 20-60% of patients.
- Less common reactions occurring in up to 2% of patients include: endophthalmitis (infectious and non-infectious), hypopyon, injection site reactions (described as blurring and transient discomfort), glaucoma, vitreous floaters, detachment of retinal pigment epithelium, optic disc vascular disorder, eye inflammation, conjunctival hemorrhage and visual acuity reduced. Cases of exophthalmos have also been reported.
- Anticoagulant Agents –Corticosteroids may enhance or diminish the anticoagulant effect of anticoagulant agents. Coagulation indices should be monitored.
- Antidiabetic Agents –Corticosteroids may increase blood glucose concentrations. Dose adjustments of antidiabetic agents may be required.
- CYP 3A4 Inducers and Inhibitors –CYP 3A4 inducers and inhibitors may respectively increase or decrease clearance of corticosteroids, necessitating dose adjustment.
- NSAIDs –Concomitant use of NSAIDS, including aspirin and salicylates, with a corticosteroid may increase the risk of GI side effects.
For additional Important Safety Information about TRIESENCE® Suspension, please see the accompanying full Prescribing Information.
References: 1. TRIESENCE Prescribing information. Harrow IP, LLC; 2023. 2. Dyer, David Md; Callanan, David Md; Clinical Evaluation Of The Safety And Efficacy Of Preservative-Free Triamcinolone (Triesence® [Triamcinolone Acetonide Injectable Suspension] 40 Mg/Ml) For Visualization During Pars Plana Vitrectomy. Retina 29(1):P 38-45, January 2009. | Doi: 10.1097/Iae.0b013e318188c6e2. 3. Thorne JE, Sugar EA, Holbrook JT, Burke AE, Altaweel MM, Vitale AT, Acharya NR, Kempen JH, Jabs DA; Multicenter Uveitis Steroid Treatment Trial Research Group. Periocular Triamcinolone vs. Intravitreal Triamcinolone vs. Intravitreal Dexamethasone Implant for the Treatment of Uveitic Macular Edema: The PeriOcular vs. INTravitreal corticosteroids for uveitic macular edema (POINT) Trial. Ophthalmology. 2019 Feb;126(2):283-295. doi: 10.1016/j.ophtha.2018.08.021. Epub 2018 Sep 27. PMID: 30269924; PMCID: PMC6348060. 4. Maia M, Farah ME, Belfort RN, et alEffects of intravitreal triamcinolone acetonide injection with and without preservativeBritish Journal of Ophthalmology 2007;91:1122-1124.